Abstract
Illicit drug and alcohol abuse by behavioral health professionals has been overlooked in psychological research. This researcher begins the analysis of substance abuse by behavioral health professionals by determining whether there is a significant difference in reported substance abuse between four categories of behavioral health professionals. The professional categories reviewed are social workers, licensed counselors, marriage and family therapists, and substance abuse counselors. Data was retrieved from the annually published Adverse Action Reports of the Arizona Board of Behavioral Health Examiners. The analysis uses a one-way ANOVA and Tukey’s post-hoc HSD test to determine the existence of a significant difference in population means of reported substance abuse by the different groups of behavioral health professionals. The researcher found that substance abuse counselors are reported for behaviors associated with substance abuse more frequently than other behavioral health professionals (F(3,18) = 4.739, p < .05). More research should be done to understand and mitigate this phenomenon.
Keywords: substance abuse, behavioral health professionals, social workers, licensed counselors, marriage and family therapists, substance abuse counselors
When people in Arizona need help recovering from their drug addiction, they are often sent to a licensed behavioral health professional to get that help. The professional they work with will probably be a Substance Abuse Counselor, someone specially trained to deal with the particular challenges of overcoming addiction. One would hope that the people hired to help those with substance abuse problems would not be in the midst of their own substance abuse problem. However, that cannot be counted on.
Defining substance abuse. The DSM-5 (2013) describes several criteria in the diagnosis of Substance Use Disorders, including but not limited to risky use of the substance in question. Behaviors that are indicative of dependency on either alcohol or illicit drugs, therefore, include those behaviors that put the individual at risk. These behaviors might be measured by their results. For example, one could count illicit drug or alcohol-related arrests, such as for driving while intoxicated, or non-criminal behaviors, such as testing positive in employment-based drug testing. Disciplinary reports could provide such a count. For that reason, this researcher defines substance abuse as the behaviors indicative of dependency on either alcohol or illicit drugs.
Current research. Although there are no studies specific to the problem of substance abuse by behavioral health professionals (BHPs) there are a number of disciplinary reports citing substance abuse policy infractions. A quick glance at the Adverse Actions Reports published in Arizona each year indicates that drugs and alcohol are problems for BHPs (Adverse Actions, 2014). However, while one can find studies of substance abuse and addiction problems in medical professionals (Domino, et al., 2005), similar studies of BHP have not happened or have not been published. Even those studies that have examined ethical challenges to the mental health field avoid substance abuse issues. A 1992 study by Pope and Vetter looked at twenty-three categories of ethical dilemmas faced by members of the American Psychological Association; Not one of those categories referenced substance abuse.
Of the behavioral health professions, only Substance Abuse Counselors (SAC) have been discussed in terms of their risk of substance abuse during their professional career. There is a history of organizations and private practices hiring recovered addicts (including recovered alcoholics) to fill that position (White, 2000). Their personal experience with addiction, it is argued, aids them as professionals because it allows for greater empathy with their clients (White, 2000). Opponents of the practice might question whether people with histories of substance abuse might increase their risk of relapse by repeatedly exposing themselves to the language and behaviors of substance abuse. One might question whether a behavioral health professional’s relapse could put their clients in danger of the same. White (2000) reported that there was a decreasing trend in the number of SAC who were themselves recovered addicts. However, his last cited estimate (62%) of SAC being recovered addicts was in 1997 (White, 2000). Currently, we do not know how many practicing SAC have a history of substance abuse, or how many have relapsed since being licensed as SAC. We also do not know whether SAC who are recovered addicts are at higher risk for substance abuse relapse than non-professionals or other BHP who have a history of substance addiction.
Indications of substance abuse. Studies on the general population give an idea of what some risk factors of substance abuse and relapse might be. The National Surveys on Drug Use and Health (Substance Abuse and Mental Health Services Administration, 2013) reported that 8.70% of Arizona residents over 26 years old, and 10.53% of Arizona residents over 18, experienced dependence on or abused alcohol or illicit drugs in 2010 and 2011. The population of behavioral health professionals in Arizona is a subset of the entire state population, so one might expect the rates of substance abuse to be similar in these populations. However, behavioral health professionals, as a group, are employed people who have self-selected into a career dedicated to helping others. This could be an indication of a tendency toward higher social responsibility, a personality trait inversely related to conscientiousness. Social responsibility combines at various life stages with social-environmental factors predict substance abuse, such that higher social responsibility predicts lower rates of substance abuse (Roberts & Bogg, 2004). Additionally, being employed increases social responsibility (Roberts & Bogg, 2004). Therefore we expect that BHP will have a lower substance abuse rate than their peers not in the same career category.
Sinha (2001) found stress to be a factor in relapses. As a group, BHP are subjected to vicarious traumas and lesser negative experiences, compassion fatigue, and general stress (Adams, Boscarino, & Figley, 2006). Additionally, behavioral health professionals are unlikely to seek out help when stress becomes overwhelming (Siebert & Siebert, 2007). These factors (high stress and reluctance to seek help) could increase their risk for substance abuse, particularly for those BHP with a history of substance abuse, for whom relapse is a possibility. If Substance Abuse Counselors (SAC) are in fact more likely to have a pre-professional history of substance abuse than other BHP, then one would expect them to also have a higher risk than other BHPs of substance abuse during their employment as behavioral health professionals.
Some questions concerning the challenges specific to substance abuse by behavioral health professionals have been described. It would be helpful to understand first whether certain behavioral health professionals have greater risk for substance abuse than others. The intention of this researcher is to determine whether there is a difference in reported substance abuse between the different behavioral health professions.
Method
Data Collection
This study used archival data, and the data was freely available on the websites of the reporting agencies, which were the Substance Abuse and Mental Health Services Administration (SAMHSA), a branch of the U.S. federal government, and the Arizona Board of Behavioral Health Examiners (ABBHE). Their websites are http://samhsa.gov/ and http://azbbhe.us/, respectively. The tally and computation of data was conducted in a Microsoft Excel file.
Archives
Data for this study was retrieved from Adverse Actions Reports published by the Arizona Board of Behavioral Health Examiners (ABBHE) over the past six years (from 2008 to 2013). ABBHE Adverse Action Reports are published annually by the ABBHE, and contain records of every disciplinary (adverse) action taken in response to violations by the licensed Arizona behavioral health professionals that occur in that year.
Participants
All behavioral health professionals who practiced in Arizona during the date range between 2008 and 2013, and who were reported for adverse action during that time, are included in ABBHE Adverse Action Reports. The ages, ethnicities and genders of these participants are unknown. These reports were used to collect a tally of citations of drug and alcohol misuse by social workers in Arizona, who are licensed and regulated by the ABBHE.
Procedure
In the ABBHE Adverse Action Reports, each reported professional is listed individually, and some professionals are listed as having multiple infractions in a single incident. Some incidences are listed more than once; in these cases, adverse action reports were generated at various stages of the investigation (e.g., a report might be generated at the time of allegation, and another report might be generated at the conclusion of the investigation). This researcher tallied the number of drug or alcohol-related infractions attributed to each licensure type each year, regardless of other infractions listed in a given incident, and only tallied once for each infraction, regardless of how many times the infraction was listed. Individuals whose application for initial licensure was denied due to drug or alcohol-related infractions were included in the tally. Drug or alcohol-related infractions tallied included self-reports of substance abuse, arrests for intoxication, and positive drug test results during employment screening.
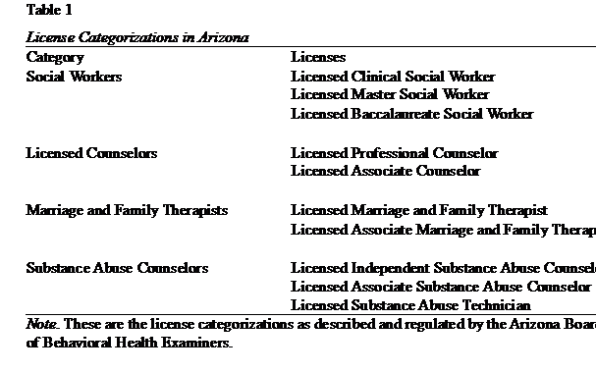
There are four categories of behavioral health professionals licensed in Arizona. These include Social Workers, Licensed Counselors, Substance Abuse Counselors, and Marriage and Family Therapists (for a list of the licenses included in each category, see Table 1, Appendix).
Tallies for drug or alcohol-related infractions were compiled in the four groups, such that all infractions for SWs were in one group, LCs in another group, MFTs another group, and SACs in another group. Drug or alcohol-related infractions included reported arrests for drug or alcohol-related crimes (e.g., drunk driving arrests), self-reported drug or alcohol dependence, and positive results on employment-based drug tests.
Finally, the researcher contacted the ABBHE by phone, and requested the total numbers of behavioral health professionals licensed in Arizona for each of the years from 2008 to 2013, and the total population of each licensure group by year. That information was given to the researcher over the phone by a qualified representative of the ABBHE.
Design
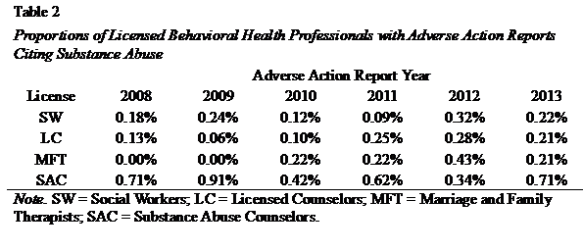
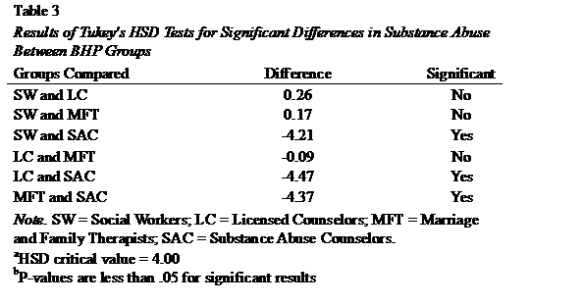
This researcher used a one-way Analysis of Variance (ANOVA) and Tukey’s Honestly Significant Difference (HSD) Test to determine whether or not there is a significant difference in the four groups’ population means of substance abuse-related adverse action reports over six years, from 2008 to 2013. The one-way ANOVA was chosen because it allowed the comparison of more than two independent groups (four independent groups were tested). Tukey’s test was used because, if there were an honestly significant difference between the groups, it could be used to determine where the difference was. The independent variable is the licensure type of the behavioral health professionals who are monitored by the ABBHE. The four groups of license types described previously make up the four levels of the independent variable. The dependent variable is the rate of drug and alcohol misuse by individuals in each group, as reported in the Adverse Action reports. The proportions of individuals cited for substance abuse in each group, in each year, are the samples (see Table 2, Appendix).
Results
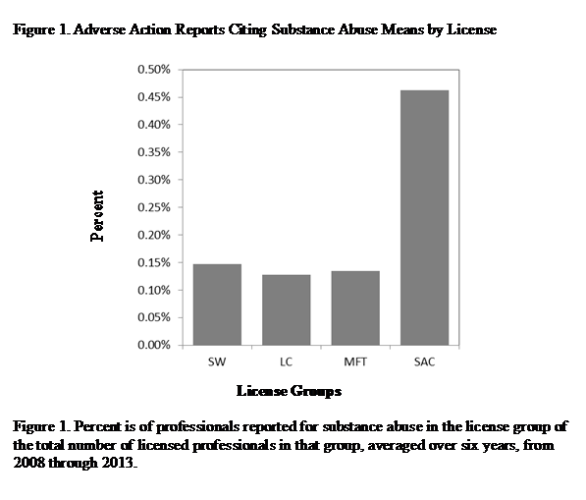
The null hypothesis is that there is no significant difference in the population means of substance abuse reported in the ABBHE Adverse Action Reports for each of the four major licensure types in Arizona. The alternative hypothesis is that there is, in fact, at least one significant difference in the population means of incidences reported in the ABBHE Adverse Action Reports for each of the four major licensure types. There was a significant difference in reported substance abuse among the Social Workers group (n = 6, M = .15%, SD = .08%), the Licensed Counselor group (n = 6, M = .13%, SD = .09%), the Marriage and Family Therapist group (n = 6, M = .13%, SD = .16%), and the Substance Abuse Counselor group (n = 6, M = .46%, SD = .21%) ( F(3,18) = 4.739, p < .05). Tukey’s HSD tests showed that the Social Workers group, Licensed Counselor group, and Marriage and Family Therapist group did not differ significantly from each other in substance abuse, but all three of those groups differed significantly from the Substance Abuse Counselor group (see Table 3, Appendix).
Discussion
This study was conducted to determine whether there is a difference in substance abuse by the different categories of behavioral health professionals, including Social Workers, Licensed Counselors, Marriage and Family Therapists, and Substance Abuse Counselors. Previous research implied a connection between substance abuse and stress (Sinha, 2001), and indicated that helping professionals such as BHP are subjected to high stress (Adams, Boscarino & Figley, 2006) but have difficulties reaching out for help (Siebert & Siebert, 2007). Further, previous research indicated that many Substance Abuse Counselors are recovered, or recovering, from substance abuse addictions and thus are at risk of relapse (White, 2000), while the same has not been indicated for other BHP. Therefore, this researcher expected to find that Substance Abuse Counselors do have a higher rate of substance abuse than do other BHP. This expectation was met.
This study was limited because it only included those BHP who were reported through ABBHE channels were included in the tally of substance abuse-related behavior. It is unknown how many BHP might behave similarly, but due to circumstance or other unidentified factors, might not have been reported for disciplinary action. A review of disciplinary actions by professional psychology boards found that many infractions are never reported (Van Horne, 2004). It is possible that behavioral health professional boards have similar inconsistencies. This study did not examine this possibility.
A potential confound of this study is that some of those reported in the Adverse Action Reports for substance abuse behaviors were applicants, as opposed to being fully licensed BHP. It is unknown whether the professionals would be more or less likely to engage in this behavior based on their status as applicants or licensees. Other potential confounds include the ages, sexes, genders, and career longevity of the BHP. None of these demographics are reported in the Adverse Action Reports, so differences based on these are unknown.
A more comprehensive study should include demographic information and a broader population. While this study included all BHP in the state of Arizona, it would be beneficial to include comparable data from other states. In addition to increasing the sample size and giving more depth to the study, this might serve to point out regional differences, which might be indicative of the relative successes of state policies on substance abuse support for BHP.
Future research should branch out from the understanding that Substance Abuse Counselors could be more likely than other behavioral health professionals to struggle with substance abuse. Studies that seek to understand the relative effectiveness of various state policies on substance abuse support for behavioral health professional should be considered, as should studies that question the risk factors for substance abuse in behavioral health professionals, such as compassion fatigue or personality types. These studies should focus particularly on Substance Abuse Counselors. It would also be beneficial to determine whether Substance Abuse Counselors who do have a history of substance addiction are more or less likely to relapse than people who have similar histories of addiction but are not behavioral health professionals.
Conclusion
It is important that people who seek help for substance use disorders are able to get help from a professional who is not at risk of succumbing to the same disorder. It is just as important that behavioral health professionals have the support required to assist clients. Substance Abuse Counselors with a history of substance abuse are common in the field, and they are attempting to help a population that does not necessarily receive a lot of empathy from others. These professionals have the empathy, they are willing to help, and they are simultaneously trying to help themselves become better people. Determining the best course of action the rest of the population can take to aid these professionals in these goals should be a priority.
References
Adams, R. E., Boscarino, J. A., & Figley, C. R. (2006). Compassion fatigue and psychological distress among social workers: A validation study. American Journal of Orthopsychiatry, 76(1), 103-108.
Adverse Actions. (n.d.) About Us. Retrieved January 29, 2014, from http://azbbhe.us/adverse-actions
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed., pp. 483-589). Substance-Related Disorders. Washington, D.C.: Author.
Domino, K. B. (2005). Risk factors for relapse in health care professionals with substance use disorders. The Journal of the American Medical Association, 293(12), 1453-1460.
Pope, K. S., & Vetter, V. A. (1992). Ethical dilemmas encountered by members of the American Psychological Association: A national survey. American Psychologist, 47(3), 397-411.
Roberts, B. W., & Bogg, T. (2004). A longitudinal study of the relationships between conscientiousness and the social- environmental factors and substance-use behaviors that influence health. Journal of Personality, 72(2), 325-354.
Sinha, R. (2001). How does stress increase risk of drug abuse and relapse? Psychopharmacology, 158(4), 343-359.
Substance Abuse and Mental Health Services Administration. (2013). 2010-2011 NSDUH State estimates of substance use and mental disorders. Retrieved February 27, 2014, from http://samhsa.gov/data/NSDUH/2k11State/NSDUHsae2011/Index.aspx
Van Horne, B. A. (2004). Psychology licensing board disciplinary actions: The realities. Professional Psychology: Research and Practice, 35(2), 170-178.
White, W. L. (2000). The history of recovered people as wounded healers: II. The era of professionalization and specialization. Alcoholism Treatment Quarterly, 18(2), 1-25.
Appendix
Agh! Such a difficult problem. I admire you for addressing it. k.